Clinical Information System
At SCC Soft Computer, we offer a cutting-edge suite of solutions designed to streamline workflows, enhance productivity, and drive breakthroughs in patient care. Our mission is to revolutionize the way laboratories operate, whether you’re part of a health system, regional hospital, public health service, commercial lab, research facility, blood management organization, or transplant medicine unit.
Enterprise Scale
- Customized modules and product suites designed to meet the unique needs of enterprise laboratories.
- Seamless integration with existing enterprise systems to streamline workflows and enhance interoperability.
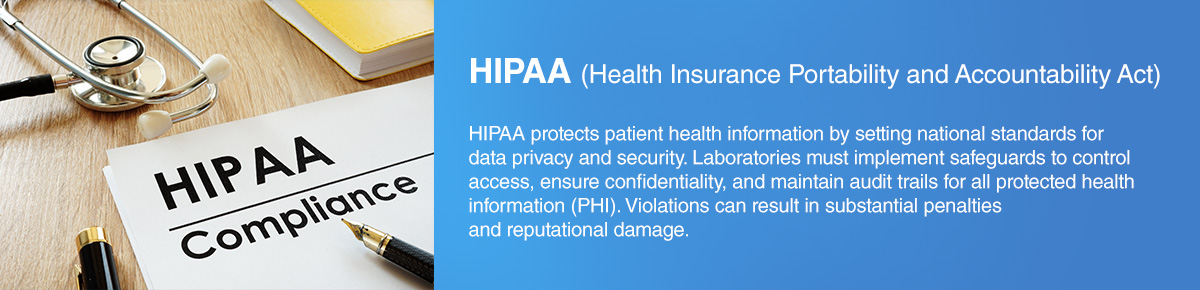
- Industry-leading security measures to safeguard sensitive laboratory data and ensure regulatory compliance.
- Dedicated technical support and comprehensive training programs.
Commercial Flexibility
- Flexible modular solutions that cater to the specific needs and budget constraints of smaller labs.
- Scalable cloud-based solutions that enable growth without significant upfront investment in infrastructure.
- Custom workflow engine to automate processes to improve operational efficiency.
- Full suite of outreach and operational solutions to improve customer service and revenue cycle management.
Driving Growth Across Diverse Industries
SCC Soft Computer is dedicated to delivering tailored solutions that enhance efficiency, accuracy, and excellence for clients across a wide range of industries, from complete healthcare systems to commercial labs.
Health Systems
Our solutions help health systems streamline workflows and improve the coordination of patient care, especially in facilities with multiple sites. By unifying systems under a single database, SCC products reduce turnaround times and facilitate seamless operation across different time zones, eliminating the need for multiple systems.
Solutions for Health Systems ›
Regional Hospitals
For regional hospitals, SCC solutions optimize resource utilization and elevate the quality of patient care. Our consistent interface design ensures a smooth user experience, while direct integration with laboratory instruments eliminates the need for middleware, simplifying operations and reducing errors.
Solutions for Regional Hospitals ›
Research
Research laboratories benefit from our solutions through enhanced data sharing and collaboration capabilities, crucial for high-volume testing environments. Our platforms perform real-time data analytics, enabling on-demand research and providing valuable insights that drive scientific discovery.
Solutions for Research ›
Commercial Laboratories
Commercial laboratories can achieve greater accuracy and efficiency in high-volume testing with SCC’s comprehensive solutions. Our LIS streamlines quality control workflows and minimizes the need for human intervention, allowing staff to focus on more critical tasks. Our integrated approach covers both the healthcare and business sides of operations, including revenue cycle management (RCM) for comprehensive operational oversight.
Solutions for Commercial Laboratories ›
Transplant Medicine
SCC Soft Computer’s solutions for Transplant Medicine provide unparalleled accuracy and efficiency, streamlining donor and recipient matching processes to ensure optimal outcomes. Our comprehensive software suite supports the entire transplant workflow, from data management and compliance tracking to real-time analytics, empowering healthcare professionals to deliver life-saving treatments with confidence.
Solutions for Transplant Medicine ›
Public Health
SCC Soft Computer’s solutions for Public Health Laboratories are designed to enhance disease surveillance, streamline testing workflows, and improve data management, ensuring timely and accurate reporting. Our robust software suite empowers public health professionals with advanced analytics and real-time monitoring capabilities, enabling them to respond swiftly and effectively to public health challenges.
Solutions for Public Health ›
Blood Management
SCC Soft Computer’s Blood Management solutions streamline the entire blood supply chain, from donor recruitment to transfusion tracking, ensuring the highest standards of safety and efficiency. Our advanced software suite offers seamless integration with laboratory systems, providing real-time data and analytics to optimize inventory management and enhance patient care.
Solutions for Blood Management ›
About SCC Soft Computer
Founded in 1979 by visionary leader Gilbert Hakim, SCC Soft Computer has established itself as a global pioneer in clinical information management systems. We specialize in providing state-of-the-art laboratory information systems (LIS) that empower healthcare organizations to optimize workflows, enhance patient care, and drive innovation. With a steadfast commitment to excellence, integrity, and customer focus, SCC Soft Computer combines cutting-edge technology with unparalleled support to deliver transformative solutions across diverse healthcare sectors. Our mission is to revolutionize healthcare by enabling laboratories worldwide to achieve unprecedented levels of efficiency and accuracy, ensuring that our clients remain at the forefront of medical advancements.
About UsClinical Information System
A clinical information system is the backbone of modern healthcare operations. It enables accurate data capture, real-time access, and integrated patient care across departments, facilities, and specialties. From medication orders to diagnostic imaging and lab results, these systems support clinicians with the structured, actionable information needed to deliver consistent, high-quality care.
Well-implemented clinical information systems in healthcare reduce redundant testing, minimize documentation errors, and accelerate treatment decisions. More importantly, they serve as unified platforms that integrate with laboratory, radiology, pharmacy, and administrative systems—creating a longitudinal patient record.
There are many clinical information system examples, including electronic health records (EHRs), clinical decision support systems (CDSS), and computerized physician order entry (CPOE) platforms. Each serves a different purpose but contributes to the same goal: reliable, secure, and efficient healthcare delivery.
At their core, all CIS platforms share fundamental architecture: secure data repositories, user authentication protocols, patient-centered interfaces, and interoperability frameworks. These components of clinical information systems ensure care teams can collaborate across time and location without compromising data integrity.
For hospitals, the benefits of a clinical information system are measurable. Fewer medication errors. Shorter lengths of stay. Better outcomes. And faster reimbursement. CIS platforms streamline administrative tasks while enhancing clinical accuracy, providing a return on investment that extends from operational efficiency to improved patient safety.
What is a Clinical Information System?
A clinical information system is a technology platform designed to collect, store, access, and manage patient health data across the continuum of care. Its primary function is to support clinical workflows while ensuring that healthcare professionals can access timely information for diagnosis, treatment, and care planning.
According to published definitions in resources such as a clinical information system PDF, these platforms combine administrative, diagnostic, and therapeutic components into a single, interoperable system. They are foundational in enabling electronic health record (EHR) functionality, diagnostic test ordering, and treatment documentation.
The role of a clinical information system in healthcare is not limited to data storage. It facilitates communication among care providers, supports evidence-based decisions, and helps standardize care delivery across departments and facilities. With rising patient volumes and regulatory demands, clinical systems are essential for ensuring operational efficiency and quality assurance.
Some commonly referenced clinical information examples include electronic medical records (EMR), computerized physician order entry (CPOE), pharmacy management systems, and clinical decision support systems (CDSS). Each is purpose-built for a specific function but integrated under the broader CIS architecture.
Understanding what is clinical information in healthcare requires distinguishing between raw data and actionable insights. Clinical information includes patient demographics, lab results, imaging studies, allergies, prescriptions, and physician notes—all structured to guide diagnosis and care planning. Without a system to manage this data, hospitals would face delays, inefficiencies, and increased clinical risk.
Key components of clinical information systems include:
- Data input modules for capturing structured and unstructured clinical data.
- Secure databases for storing and managing protected health information (PHI).
- User authentication and access control to comply with HIPAA and other regulations.
- Interoperability engines for exchanging data with labs, pharmacies, and external providers.
- Clinical documentation tools to streamline physician and nursing workflows.
When evaluating advantages and disadvantages of clinical information systems, the benefits are clear. Improved data accuracy, better care coordination, streamlined billing, and enhanced patient safety top the list. However, implementation costs, staff training requirements, and integration complexity remain significant barriers for some institutions.
Well-designed CIS platforms deliver significant value by reducing human error, accelerating workflows, and ensure care teams have the full clinical picture at every touchpoint. The ability to document once and share across systems reduces duplication and supports better decision-making.
What is an Example of a CIS in Healthcare?
Understanding real-world examples of clinical information systems in healthcare reveals how essential these platforms are in delivering efficient, compliant, and coordinated care. A CIS system in healthcare is not a single application—it’s a framework of integrated tools that work together to support clinicians, laboratory personnel, radiologists, pharmacists, and administrative teams.
One clear example is the electronic health record (EHR) system. EHRs centralize patient medical histories, lab results, prescriptions, and clinical documentation. They allow authorized users across departments to access updated health information in real time. This capability reduces communication delays and prevents redundant testing—key drivers of patient safety and cost control.
Another example is computerized physician order entry (CPOE). This tool allows providers to enter medication orders, lab requests, and imaging studies directly into the system. The orders are immediately routed to the correct department, eliminating errors caused by handwritten notes or verbal communication. Many CPOE platforms also include built-in clinical decision support to warn providers of drug interactions, dosage errors, or contraindications.
Laboratory information systems (LIS) are also key components of clinical information systems. These manage specimen handling, test processing, result reporting, and instrument integration within the lab. A well-integrated LIS feeds results back to the EHR, enabling providers to view real-time lab data alongside clinical notes and imaging reports.
What ties all these components together is their alignment with the broader purpose of a CIS: delivering timely, accurate, and secure clinical data to the right person at the right time. The system enables clinical collaboration, supports patient safety protocols, and ensures documentation meets regulatory and reimbursement requirements.
When considering what are 3 types of clinical information, they generally fall into these categories:
- Administrative data – Patient demographics, scheduling, and billing.
- Clinical documentation – Progress notes, assessments, and care plans.
- Diagnostic data – Laboratory results, imaging, and pathology reports.
Each of these types must be integrated and accessible across care settings to provide a complete picture of patient health. Without integration, care is fragmented, outcomes suffer, and operational costs increase.
The best clinical information system in healthcare environments is one that supports modular integration, role-based access, system-wide alerts, and data normalization—ensuring consistency across clinical, diagnostic, and administrative domains.
What are 3 Types of Clinical Information Systems?
There are three primary categories of clinical information systems used across hospitals and health networks, each aligned to a different layer of patient care and institutional management. These categories reflect how data flows through a healthcare environment—capturing, processing, and acting on information from intake through treatment and beyond.
- Electronic Health Record (EHR) / Electronic Medical Record (EMR) Systems
These systems serve as the core clinical documentation platforms. They contain patient medical histories, encounter notes, medication lists, allergies, immunizations, vital signs, and care plans. EHRs are often the central hub through which other systems—such as LIS, PACS, and CPOE—communicate. - Clinical Decision Support Systems (CDSS)
CDSS tools analyze clinical data and provide prompts or alerts to assist providers in making evidence-based decisions. For example, a CDSS may issue warnings about drug interactions, recommend diagnostic tests based on symptom profiles, or support treatment protocol adherence. These systems reduce variation in care and improve patient outcomes. - Computerized Physician Order Entry (CPOE) Systems
These platforms allow clinicians to electronically enter orders for medications, labs, and imaging. Integrated with CDSS, they help catch dosage errors, prevent contraindicated prescriptions, and eliminate communication gaps between ordering and fulfillment departments.
Together, these represent the dominant types of healthcare information systems in use. However, they exist alongside other subsystems that support specific domains such as pharmacy, nursing, and radiology information systems.
The types of health information systems PDF documents available from academic and government sources often expand these categories to include:
- Administrative systems, such as billing, registration, and scheduling.
- Data warehouse systems, which aggregate data from multiple sources for analytics.
- Mobile health (mHealth) platforms, enabling remote monitoring and patient engagement.
Each of these systems can be classified under broader types of hospital information system categories that include both clinical and administrative components.
Understanding system classifications helps clarify how information flows between care settings. For example, a LIS feeds diagnostic data into the EHR, which is then used by a CDSS to generate alerts, all while administrative systems manage coding and billing for the same encounter.
The integration between administrative information systems in healthcare and clinical systems is significant in value-based care environments. By linking patient outcomes to resource utilization and reimbursement, integrated systems enable data-driven decision-making that benefits both patients and providers.
The clinical information system benefits in this context are substantial:
- Improved patient safety through decision support and standardized workflows
- Faster communication between departments
- Reduced redundancies in testing and documentation
- Stronger compliance with regulatory frameworks
- Enhanced reporting capabilities for internal audits and external accreditation
By choosing systems that align with these categories and integrating them properly, healthcare organizations can achieve comprehensive visibility, operational control, and sustainable clinical performance.
Is CIS the Same as Information Systems?
Is CIS the same as information systems in computer science or business technology? No—although they share structural similarities, a clinical information system (CIS) is a specialized subset of broader information systems designed explicitly for healthcare settings.
In a general context, computer information systems manage data for a variety of organizational functions: finance, logistics, customer relationship management, and more. These systems focus on information flow, data security, analytics, and clinical laboratory automation across industries. Their core competencies include database architecture, network design, and enterprise resource planning.
By contrast, a clinical information system in healthcare is tailored to the clinical environment. It deals explicitly with patient records, treatment data, clinical workflows, and healthcare compliance. Its focus is not just data management, but the safe and timely delivery of patient care, governed by medical protocols and regulatory mandates.
A professional with a computer information systems degree may find employment across multiple sectors, including healthcare, but they would need additional domain expertise to manage CIS platforms effectively. Healthcare-specific standards such as HL7, FHIR, and HIPAA compliance are central to CIS but not typically emphasized in general information systems curricula.
The overlap between CIS and other IT systems lies in architecture and technology—databases, user interfaces, integration engines—but diverges significantly in application and compliance requirements. For instance, a general database administrator may not have the clinical context to design a medication order entry interface or manage patient consent tracking.
In terms of career pathways, computer information systems jobs in healthcare often require cross-functional skills. Employers seek professionals who can bridge the gap between IT operations and clinical practice. This includes roles such as clinical systems analysts, health informatics specialists, and EHR implementation consultants—positions demanding fluency in both technical platforms and healthcare workflows.
In summary, while all CIS platforms are information systems, not all information systems are CIS. Clinical information systems are a specialized category, purpose-built for managing and improving patient care. Their success depends not only on IT competency but on clinical awareness, regulatory alignment, and user-centered design.
Choosing the Right LIS
Selecting the right laboratory information system requires a close match between software capabilities and the laboratory’s operational needs. SCC’s SoftLab® delivers advanced sample tracking, real-time data integration, and full compliance with regulatory requirements—making it an ideal choice for clinical labs embedded within broader healthcare information systems.
The best LIS software supports multi-instrument workflows, audit-ready documentation, and seamless interoperability with EHR, billing, and diagnostic platforms. SoftLab is built for performance, scalability, and reliability—enabling labs to process high volumes of data without sacrificing accuracy or speed.
For healthcare organizations that rely on precise, efficient laboratory operations to inform clinical decision-making, SoftLab offers the control, flexibility, and system-wide integration that modern environments demand.