Key Takeaways
- A clinical information system is designed to manage and present clinical data used directly in patient care activities.
- These systems support clinicians by organizing patient information, test results, and clinical documentation in a structured manner.
- Clinical information systems are often integrated with other healthcare systems to enable consistent data exchange across departments.
- Proper use of these systems improves workflow efficiency, data accuracy, and clinical decision-making.
- Clinical information systems also support compliance, reporting, and quality monitoring within healthcare organizations.
In medical contexts, a clinical information system (CIS) is a digital framework designed to manage, store, and deliver patient-related data in real time across departments. Central to modern healthcare operations, enabling timely coordination and evidence-based care. The CIS acts as the connective tissue between clinicians, diagnostics, pharmacy, and administrative teams.
The core components of a clinical information system include:
- Data acquisition and input (clinical notes, vitals, orders)
- Data storage and retrieval (databases with structured/unstructured content)
- Clinical decision support (real-time alerts and evidence-based recommendations)
- Communication modules (messaging, interface engines, interoperability protocols)
- Workflow and audit management (routing, access control, and time-stamping)
CIS platforms function within hospitals, outpatient clinics, and labs, ensuring every care decision is backed by accurate, accessible patient data. By design, they must support integration with electronic health records (EHRs), laboratory information systems (LIS), computerized physician order entry (CPOE), and imaging archives (PACS).
The clinical information system benefits are measurable. CIS platforms reduce duplication of tests, prevent medication errors, streamline documentation, and support regulatory compliance through detailed audit trails. They also enhance communication between departments, minimize delays in care, and improve data security through role-based access and encryption protocols.
As hospitals expand their digital infrastructure, the CIS remains central to achieving clinical accuracy, patient safety, and operational efficiency. It is not merely a tool for documentation—it is a clinical asset that actively shapes patient outcomes through real-time, system-wide data visibility.
What are 3 Types of Clinical Information Systems?
While the term clinical information system refers broadly to platforms managing patient care data, it comprises specific subsystems with distinct purposes. The three foundational types—electronic health records, practice management systems, and health information exchanges—form the operational backbone of most healthcare environments.
Electronic health records (EHRs) are the primary system for clinical documentation and patient data storage. EHRs house structured inputs such as vital signs, lab results, allergies, medications, diagnostic images, and treatment histories. These records are accessible by authorized clinicians across the continuum of care, enabling accurate, up-to-date decision-making at every stage of treatment.
Practice management systems (PMS) support the administrative side of care. While not always labeled as clinical, they play a critical role in linking patient data to appointments, billing, insurance claims, and resource allocation. Integration with EHRs ensures smooth coordination between front-desk operations and clinical workflows.
Health information exchanges (HIEs) serve a regional or national purpose—enabling the secure sharing of patient information across disparate healthcare systems. HIEs pull relevant clinical data from various providers, offering a unified patient view to emergency departments, specialists, and labs outside the originating system. This reduces redundancy, flags potential medication conflicts, and enhances care continuity when patients transition between facilities.
Each of these systems is considered part of a broader clinical information system infrastructure because they contribute to data accuracy, clinical insight, and operational efficiency. When EHRs, PMS platforms, and HIEs function in sync, healthcare organizations can provide consistent, compliant, and coordinated care—regardless of scale or location.
Clinical Information Examples
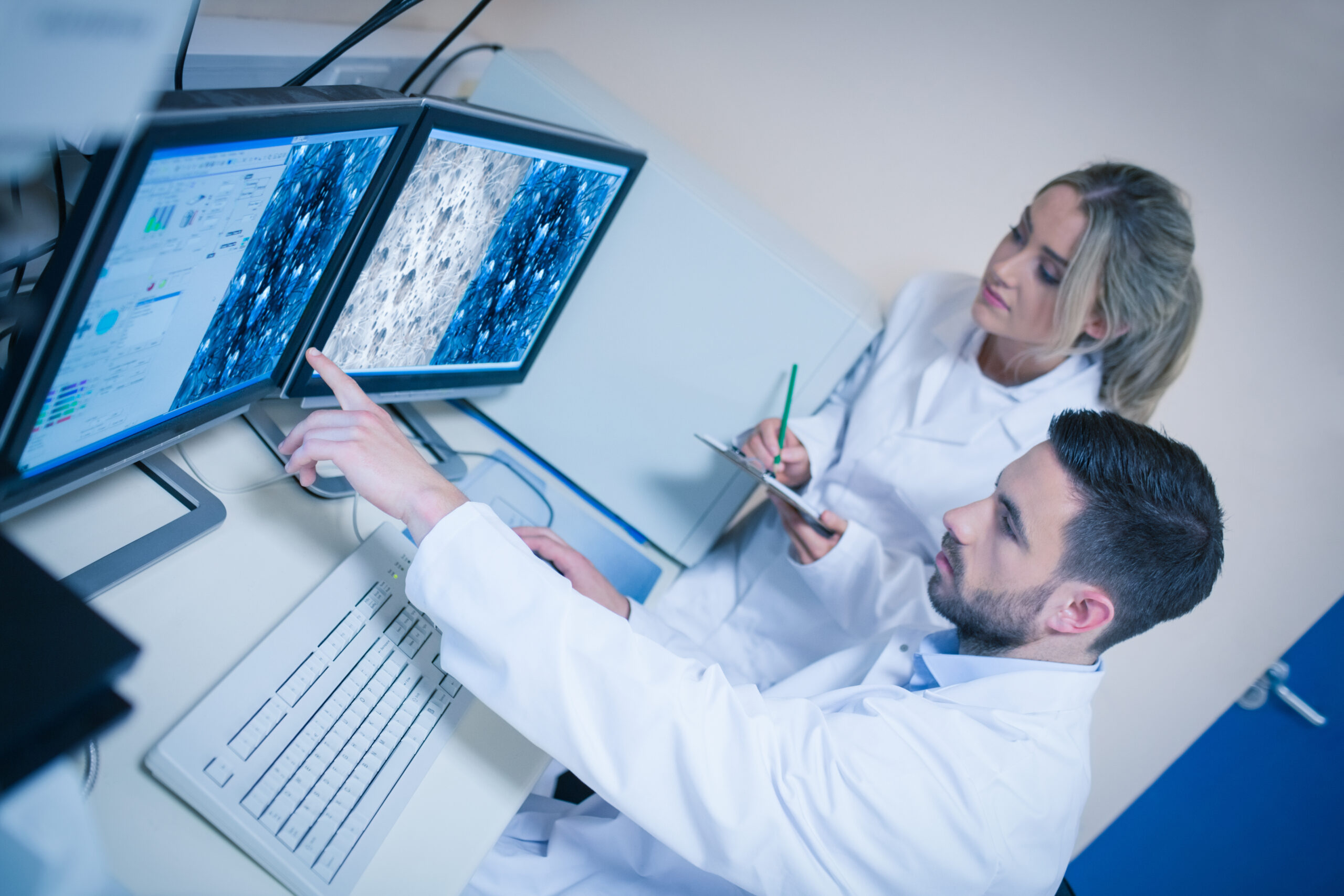
To fully understand the role of a clinical information system, it’s essential to explore how clinical data is captured, categorized, and applied. Practical examples of clinical information systems in healthcare include electronic health records (EHRs), laboratory information systems (LIS), and radiology information systems (RIS). Each collect and distributes specific data to support care delivery.
The 2 types of medical data most often managed within these systems are structured and unstructured data. Structured data includes predefined fields such as lab values, diagnostic codes, medication dosages, and timestamps. It is ideal for analytics, alerts, and automated workflows. Unstructured data, on the other hand, consists of free-text clinical notes, operative reports, or patient narratives. While harder to parse computationally, unstructured inputs offer clinical nuance and context not captured in checkboxes or dropdown menus.
Within a hospital setting, types of clinical data extend across specialties and departments. In a lab, data may include test requisitions, analyte values, and specimen status. In imaging, radiologists capture modality-specific interpretations, measurements, and procedural metadata. Nurses document vitals, interventions, and shift reports. These inputs are tied to the patient’s longitudinal health record, accessible through the CIS.
These examples illustrate the diversity of data that must be stored, retrieved, and interpreted accurately. A radiology report linked with medication history may trigger a contraindication alert. A pathology result might update a diagnostic code or clinical staging entry. In each case, the clinical information system ensures timely, secure, and coordinated access to these details.
Without centralized systems to manage information, errors increase, and clinical decision-making slows. These data categories—and the systems that manage them—form the informational core of modern healthcare delivery.
Choosing the Right LIS
Selecting a laboratory information system that aligns with broader clinical infrastructure is critical to diagnostic accuracy and system-wide efficiency. SCC’s SoftLab® is engineered to integrate seamlessly with hospital CIS platforms, ensuring lab data flows directly into clinical workflows without delay or data loss.
The best LIS software should do more than manage samples and results—it must support multi-site operations, regulatory compliance, automation, and real-time interoperability. SoftLab enables labs to maintain tight control over test routing, instrument interfaces, and quality checks, while meeting CAP, CLIA, and HIPAA standards.
For healthcare organizations demanding precision, speed, and EHR integration, SoftLab delivers dependable performance as part of a fully interoperable clinical ecosystem.