Key Takeaways
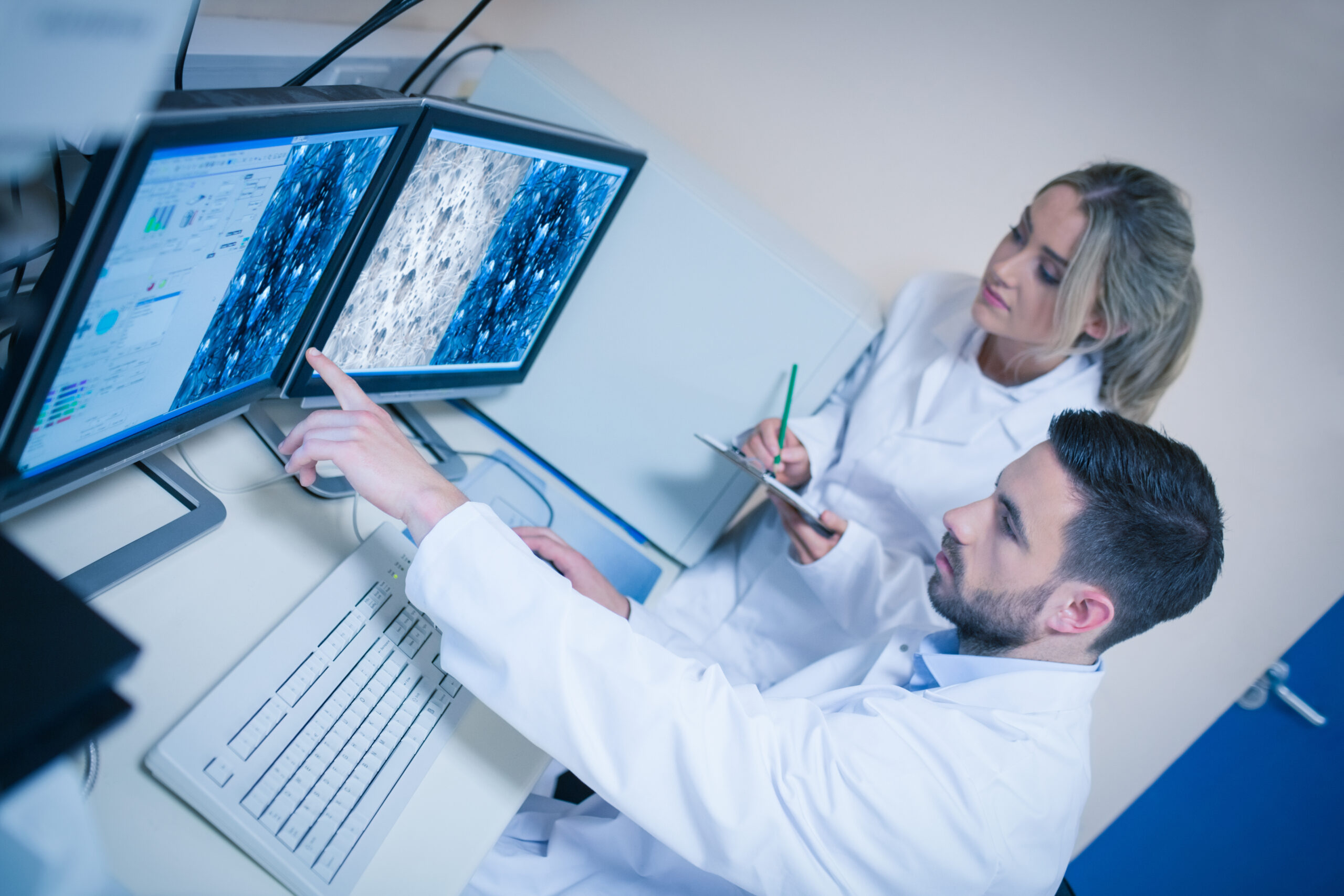
- Clinical information systems are used to manage data that supports direct patient care and clinical decision-making.
- One common type focuses on patient records and clinical documentation to provide a comprehensive view of patient history.
- Another type supports diagnostic and laboratory workflows by managing test orders, results, and related clinical data.
- A third type provides decision support by helping clinicians interpret data and apply clinical guidelines.
- Together, these systems improve care coordination, accuracy, and efficiency across healthcare environments.
A clinical information system (CIS) is a digital platform used to manage patient health data across various departments and clinical functions. Rather than existing as a single tool, a CIS is composed of multiple integrated subsystems tailored to different aspects of care. These subsystems fall into three primary categories within the broader types of healthcare information systems.
- Electronic Health Records (EHRs)
EHR systems are the core of most CIS environments. They store patient demographics, clinical notes, medication lists, allergies, immunizations, and past medical histories. EHRs enable authorized users—physicians, nurses, pharmacists, and administrators—to access and update a unified patient record in real time. They also support interoperability with labs, imaging centers, and pharmacies. - Computerized Physician Order Entry (CPOE)
CPOE systems allow providers to enter treatment instructions electronically, replacing paper orders or verbal communication. These systems reduce medication errors, standardize order workflows, and integrate with decision support tools. CPOE is often linked to pharmacy, radiology, and laboratory systems—making it a central function in many hospital settings. - Clinical Decision Support Systems (CDSS)
CDSS tools enhance diagnostic accuracy and treatment consistency by delivering real-time alerts, reminders, and evidence-based recommendations. These systems analyze current patient data against clinical guidelines and issue prompts about drug interactions, abnormal results, or missed interventions.
Together, these systems define the most common types of hospital information systems in clinical practice. While administrative systems manage scheduling and billing, CIS platforms are exclusively focused on clinical workflows—diagnosis, treatment, monitoring, and outcome analysis.
Each of these systems must communicate fluidly with one another to avoid silos, redundancies, and delays. When properly integrated, they deliver the clinical insight needed for safe, efficient, and data-driven care.
What Are The 3 Types of Clinical Information?
In any healthcare setting, information is only useful when it’s structured, categorized, and accessible. A clinical information system must handle multiple data types to support diagnosis, treatment, and administrative coordination. The three types of clinical information—patient data, medical knowledge, and directory information—form the foundation of all clinical decisions and healthcare operations.
- Patient Data
This includes all information specific to an individual patient. It spans demographics, vital signs, lab results, medication history, allergies, diagnostic imaging, and progress notes. Patient data is the most frequently accessed category in daily care and must be consistently updated and securely stored. Clinical staff depend on this data to monitor patient status, assess outcomes, and adjust treatment plans. - Medical Knowledge
This data type encompasses the clinical guidelines, protocols, pharmacology databases, diagnostic criteria, and evidence-based practices embedded in decision support tools. It allows a clinical information system to do more than store data—it provides a framework for recommending interventions, flagging adverse drug interactions, and aligning care with best practices. - Directory Information
Directory information includes internal reference data such as provider directories, departmental contacts, procedural codes, lab test definitions, and institutional policies. It supports workflow consistency, enforces standards, and helps route orders and communications to the correct individuals or systems.
A robust CIS must be configured to handle these distinct categories without blending or misclassifying data. This structure ensures frontline users access the right information in the correct context. For example, retrieving patient data without current medical knowledge (e.g., treatment protocols) creates risk. Similarly, incorrect directory information can delay orders or cause miscommunication between departments.
Ultimately, CIS performance depends not only on system speed or interface design but on its ability to manage all three types of clinical information in a way that supports safe, efficient, and compliant care delivery.
Clinical Information System Benefits
The value of a clinical information system extends well beyond data storage. These systems transform how clinical teams operate—accelerating decisions, reducing manual errors, and supporting care coordination at scale. The most widely recognized clinical information system benefits arise from their ability to centralize, standardize, and distribute medical data across departments and provider roles.
First, CIS platforms ensure seamless access to comprehensive patient records. Providers no longer rely on faxes, verbal reports, or handwritten notes. Instead, lab results, imaging findings, medication lists, and vital signs are available in one interface—improving the accuracy and speed of diagnosis.
Second, these systems are designed for interoperability. They integrate with laboratory systems, pharmacy platforms, and radiology tools to provide consolidated clinical insight. This eliminates the delays and redundancy caused by disconnected data silos. Many of the examples of clinical information systems in healthcare, such as EHRs and CPOE systems, are built around this unified access model.
According to a well-structured clinical information system PDF used in health IT training, CIS platforms also enhance compliance. Features such as electronic audit trails, secure messaging, and decision support ensure organizations meet standards set by HIPAA, CLIA, and CMS without overburdening staff. For institutions undergoing accreditation or quality audits, this is especially important.
A high-performing CIS incorporates key components of clinical information systems, including:
- Clinical documentation tools
- Data integration engines (e.g., HL7, FHIR)
- Decision support modules
- Workflow automation frameworks
- Reporting and analytics dashboards
Each of these components contributes to reduced administrative overhead, better population health tracking, and real-time care optimization.
Understanding clinical information examples further highlights the breadth of data CIS manages that includes structured inputs such as lab values and medication dosages, as well as unstructured data like clinical notes or consult summaries. By capturing and organizing both, CIS ensures a comprehensive clinical narrative is preserved.
Finally, the answer to what is clinical information in healthcare lies in its usability. Data has no value unless it informs decision-making. CIS are engineered platforms to turn disparate inputs into clear, actionable insights—ensuring better outcomes for patients and operational control for healthcare organizations.
Choosing the Right LIS
For hospitals and laboratories operating within a CIS framework, selecting the right laboratory information system is critical. SCC’s SoftLab® is engineered to meet the needs of high-volume clinical environments by ensuring fast, accurate diagnostics and end-to-end sample management.
The best LIS software integrates seamlessly with EHRs, CPOE systems, and clinical decision support tools. SoftLab offers real-time result reporting, multi-site support, and audit-ready documentation—all while complying with industry standards such as CLIA, CAP, and HIPAA.
Labs that require precision, speed, and regulatory alignment benefit from SoftLab’s configurable workflows and proven performance within larger CIS ecosystems.