Key Takeaways
- LIMS are used to capture patient test results directly from instruments or through controlled manual entry, reducing transcription errors.
- Results are stored in a centralized system that supports traceability, versioning, and long-term record retention.
- Review and verification workflows help ensure patient results are accurate and approved before release.
- Role-based access and security controls protect sensitive patient information and limit unauthorized access.
- Built-in audit trails document changes and actions, supporting accountability and compliance requirements.
A laboratory information management system functions as the central repository for managing, validating, and storing clinical results. From specimen accessioning to final report delivery, every data point is captured, timestamped, and traceable. LIMS software enforces quality and regulatory standards by structuring data input, automating result verification, and maintaining a permanent audit trail of all user actions.
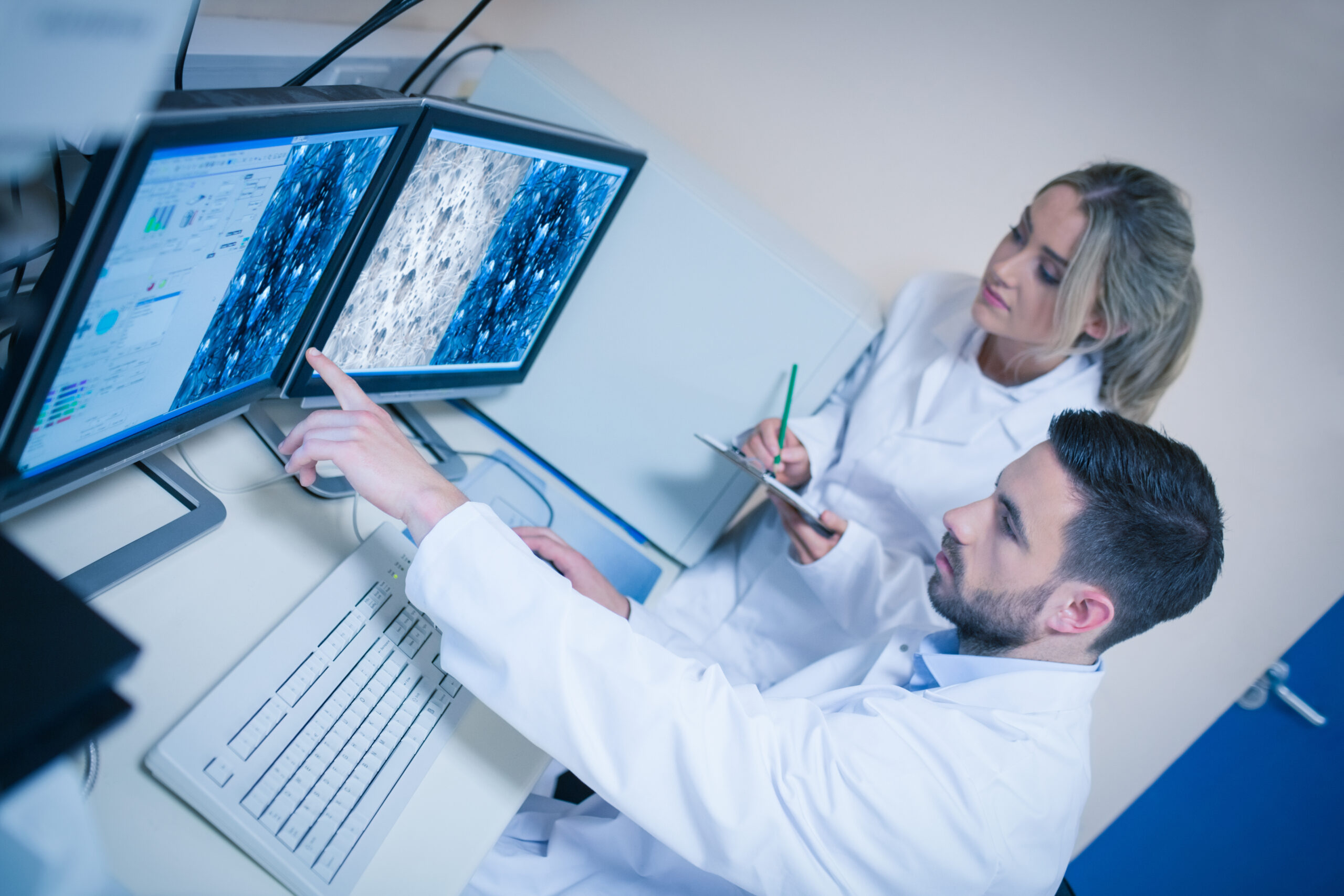
Results generated by analyzers interface directly with the LIMS system software, which applies rules-based logic to flag abnormal findings, initiate reflex testing, or halt verification pending review. This reduces the risk of manual error and ensures data integrity throughout the testing cycle.
Each patient’s result history is stored with version control, allowing laboratories to retrieve prior values for delta checks or longitudinal analysis. Secure role-based access ensures compliance with HIPAA and institutional policies, allowing only authorized users to view or modify records.
Once validated, results are transmitted through HL7 interfaces to electronic health record systems, external providers, or reference clients. This seamless communication supports both inpatient and outreach models, preserving result fidelity while minimizing transcription risk.
Beyond data capture, a laboratory information management system also supports regulatory requirements through integrated QC tracking, audit-ready documentation, and real-time monitoring of turnaround times. These capabilities enable laboratories to meet service-level agreements while maintaining strict compliance with CLIA, CAP, and other governing bodies.
LIMS usage in patient result management centers on structured workflows, automated validation, secure data storage, and full traceability. These components form the backbone of reliable diagnostic reporting in modern clinical laboratories.
LIMS Examples
Understanding how laboratories use LIMS begins with visualizing workflows and examining practical applications. A complete LIMS workflow diagram depicts specimen intake, test assignment, instrument interfacing, result validation, and final reporting—each stage governed by configurable rules. These diagrams aren’t theoretical. They reflect real-world implementations where automation reduces manual effort and enforces regulatory compliance.
One common example is in clinical chemistry labs, where LIMS auto-verifies results within defined ranges, flags exceptions for manual review, and routes confirmed data to the LIS or EHR. In microbiology, the system tracks culture stages, organism identification, and susceptibility profiles, managing dependencies without user intervention. Anatomic pathology modules route digital images and structured reports to pathologists while ensuring standard nomenclature and report templates are followed.
LIMS advantages and disadvantages become clear during implementation. Advantages include centralized data access, reduced transcription errors, faster turnaround times, and improved audit readiness. Disadvantages emerge when systems are poorly configured, overly rigid, or mismatched to lab type. Common missteps include forcing generic workflows onto specialized disciplines or underestimating the training required to replace legacy processes.
Highlighting the disadvantages of LIMS reinforces the importance of selecting systems with adaptable configuration tools. Labs using vendor-locked platforms often struggle to adjust workflows internally, leading to expensive change orders and operational bottlenecks. Another frequent issue involves failed integrations—particularly with older instruments or non-standard EMR platforms—which force staff into manual entry or external tracking tools.
LIMS usage must match the lab’s operating model. Labs with high-volume, standardized workflows will see different benefits and challenges than specialty environments like cytogenetics or toxicology. Evaluating vendor-provided diagrams, training protocols, and customer success stories helps clarify how a LIMS will function in your environment—not just in theory.
LIMS Limitations
Even advanced systems have constraints. Functionality gaps, poor scalability, and rigid configurations are among the most cited limitations in post-implementation reviews. A laboratory information management system must align not just with current operations but with how a lab evolves over time. If the system fails to support new workflows, integrate emerging instruments, or accommodate regulatory updates, it will become an operational liability.
This becomes especially critical when evaluating which of the following are features of the LIMS that support management of laboratory operations? Common expectations include real-time specimen tracking, quality control monitoring, automated reporting, integration with billing, and EHR platforms. When these features are absent or non-configurable, labs are forced to develop workarounds that compromise efficiency and compliance.
Another limitation arises from modular architecture. Systems that segment key functions into separate interfaces create user friction and require repeated logins, duplicate data entry, and fragmented reporting. A unified platform with shared data and interface consistency avoids these disruptions.
Some systems also lack configurability at the role level. When every user sees the same interface regardless of job function, productivity suffers. The best LIMS platforms present users with role-specific dashboards, task queues, and alerts—streamlining the interface to match job responsibilities.
Data migration is another common pain point. Legacy system data often lacks structure, making conversion to modern formats time-consuming and error-prone. Without dedicated support and validation tools, historical data can be lost or rendered inaccessible.
Finally, poor vendor responsiveness amplifies all technical limitations. When support delays compound system issues, labs face prolonged downtime, missed SLAs, and audit risks. A feature-rich system that lack active vendor engagement is no better than an outdated platform.
Choosing the Right LIMS
SoftLIMS delivers more than baseline functionality—it supports lab growth, automation, and compliance without adding complexity. Unlike generic systems, it adapts to clinical, pathology, or molecular environments without custom development cycles.
The best LIMS software provides long-term sustainability through scalable architecture, built-in integration capabilities, and responsive support. Labs should prioritize vendors that offer transparent upgrade paths, regulatory alignment, and role-specific configuration options.
SCC Soft Computer’s SoftLIMS reflects this standard, giving labs a configurable foundation that evolves with operations and regulatory demands.